Skills Video Drawing Blood From an Picc
See also
Procedural pain management guideline
Peripheral Intravenous device management guideline
RCH comfort kids resources
Key points
- Anxiety, pain, distress and subsequent needle phobia is associated with repeated attempts at intravenous access; appropriate preparation can minimise the distress caused.
- It is important to justify the need for the procedure and combine with blood sampling if needed.
- If available, ultrasound guidance should be considered if intravenous cannulation is predicted to be difficult or prolonged therapy is anticipated.
- Some children are at higher risk of decompensation with multiple IV attempts, e.g. child with congenital heart disease and single ventricle physiology.
Background
Multiple attempts at IV insertion can cause significant distress for patients so alternatives to IV access should always be considered within the clinical context e.g. Oral or NG fluids/medication, IM or IO medications in emergencies.
Cannulas inserted over joints, in areas of flexion or in the lower limb are more likely to fail than those inserted in the hand or forearm
Selection of Intravenous (IV) access
The following guidelines should be considered when referring patient for IV access
| Duration IV access required | Selection of cannula |
| <7 days | Peripheral IV access Predicted dwell time: forearm > hand > foot > cubital fossa Ultrasound guided peripheral IV access (may last up to 7 days) |
| 7-14 days or failed peripheral IV attempts | Upper arm midline, PICC (peripherally inserted central catheter) or Percutaneous CVAD (Central Venous Access Device) |
| >14 days / longer term | PICC, percutaneous CVAD, consider tunnelled (surgical) CVAD or port |
If available, ultrasound guidance should be considered if intravenous cannulation is predicted to be difficult or prolonged therapy is anticipated (see table below)
Potential Complications
- Accidental arterial cannulation
- Consider intra-arterial cannulation if
- Bright red backflow of blood into IV cannula
- The cannula flashback appears pulsatile or there is pulsatile movement of blood in IV tubing
- Backflow of blood into IV tubing despite fluid bag at level higher than IV insertion site
- IV inserted in a "high risk" area i.e. antecubital fossa
- Management if uncertain
- Do not use cannula
- Urgent blood gas analysis from inserted cannula
- Consider intra-arterial cannulation if
- Extravasation injury
- Needle stick injury
- Thrombophlebitis / infection
- Unsuccessful procedure
Equipment, Analgesia, Anaesthesia and Sedation
| The patient | Infants <3 months
Older infants & children
|
| Setting & equipment |
Have equipment ready before the child enters the room
Additional equipment if performing ultrasound guided intravenous cannulation
|
| Yourself |
|
Procedure
Explain the procedure to the child and parents and obtain verbal consent.
Sites
- Look carefully with a tourniquet for the most suitable vein; in children, the most suitable vein may not necessarily be palpable
- Dorsum of the non-dominant hand is preferred - the vein running between the 4th and 5th metacarpals is most frequently used
- In addition to the usual sites in adults, commonly used sites in children include the volar aspect of the forearm, dorsum of the foot and the great saphenous vein at the ankle
- Consider practicalities of splinting (eg elbow, foot in a mobile child)
Transillumination
- Application of a COLD light directly to the skin in a darkened room can be helpful in finding veins in neonates and infants
- Only cold lights (usually fibre-optic sources) should be used. Normal torches can burn the skin and should never be used
- Trans-illumination adds a layer of complexity to IV insertion as the operator has to hold a light to the skin, position the site and insert the cannula
Ultrasound guided approach
- Scan carefully for the most suitable vein
- The most commonly used vein with the highest success rate in children is the cephalic vein in the proximal forearm
- Other sites include the long saphenous vein at or just proximal to the ankle, or the medial aspect of the upper arm (midline catheter)
Assess difficulty of intravenous cannulation
- History of 'difficult' IV access in the medical record
- Patient or caregiver reports a history of difficulty in cannulating or venepuncture
- Clinical assessment. The DIVA (Difficult Intravenous Access) score may be helpful
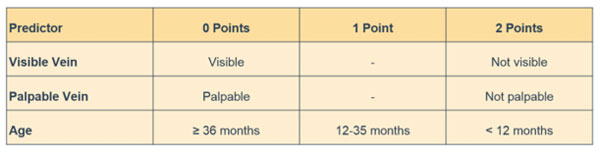
Score of 4 or more means >50% chance of failed initial attempt
If difficult intravenous cannulation is predicted based on the above criteria, ultrasound guided insertion should be considered if the equipment and expertise is available.
Some children are at higher risk of decompensation with multiple IV attempts, eg congenital heart disease with single ventricle physiology. If >2 attempts are required involve the senior clinician and consult the treating cardiology team.
Technique
Holding
- Ask assistant to stabilise limb, by holding joints above and below if necessary
- If applying tourniquet, be careful not to pinch skin or compress artery
- In infants, when accessing the hand, grasp as shown; this achieves both immobilisation and tourniquet (Figure 1 below)
Inserting the cannula
- Decontaminate skin with alcohol 70% / chlorhexidine 2% swabs and leave to dry for at least 30 seconds. Use 'no-touch' technique for insertion after decontamination
- Insert just distal to and along the line of the vein
- Angle at 10-15° (Figure 2 below), or between 30-45° if using ultrasound guidance
- Advance needle and cannula slowly
- A 'flash back' of blood may not occur for small veins and 24G cannula
- Once in vein, advance the needle and cannula SLOWLY a further 2-3mm along the line of the vein before advancing cannula off needle
- Secure the hub of the cannula at the skin entry point either by holding it down or asking the assistant to place tape across
- Dispose of sharps appropriately
Taking blood samples
- For 24G cannula, it is often easier to let blood drip passively into collection bottles (Figure 3 below)
- When taking blood for culture or gas from small cannula, aspirate blood from the hub of the cannula using a blunt 'drawing up' needle and syringe (Figure 4 below)
- For larger cannula, a syringe can be used to aspirate blood or a vacuum connector for cannulae 22G and larger
 |  |
| Figure 3: passive blood collection for infants | Figure 4: aspirating blood for culture or gas |
Securement
- Remove tourniquet before strapping
- Connect the saline-primed 3-way connector to the end of the cannula by screwing it firmly on. Flush the connector tubing with more saline to confirm intravenous placement
- Use sterile tapes to secure the hub and a clear dressing over the cannula site such as Tegaderm™. Ensure that the proximal tip and area of skin around are always easily visible (Figure 5 below). Extravasation injuries can occur especially if the site is not readily accessible for regular nursing checks
- Consider placing a small piece of cotton wool ball or gauze underneath the hub of the cannula to prevent pressure areas
- Tapes and splint should secure the limb proximal and distal to the cannula (keeping thumb free) but not too tightly (Figure 6 below)
- Arm splints are not required for lines placed in the cephalic vein in the forearm (typically ultrasound guided). Cover the whole distal extremity in net bandage (eg surgifix tubular-fast). In very young children, consider bandaging the other hand as well to prevent them from removing the cannula
Post-Procedure Care
- Running a 'drug line' (3-5ml/hr of Sodium Chloride 0.9%) through the cannula may keep it patent for a longer period of time
- Regularly inspect insertion site for complications (tenderness, blockage, inflammation, discharge) - check the other hand if it has also been bandaged
- Unless complications develop, the peripheral IV should remain insitu until IV treatment complete
Difficulty with IV insertion
Each clinician should have a maximum of 2 attempts before escalating.
Strongly consider ultrasound assistance, if available, after 3-4 attempts
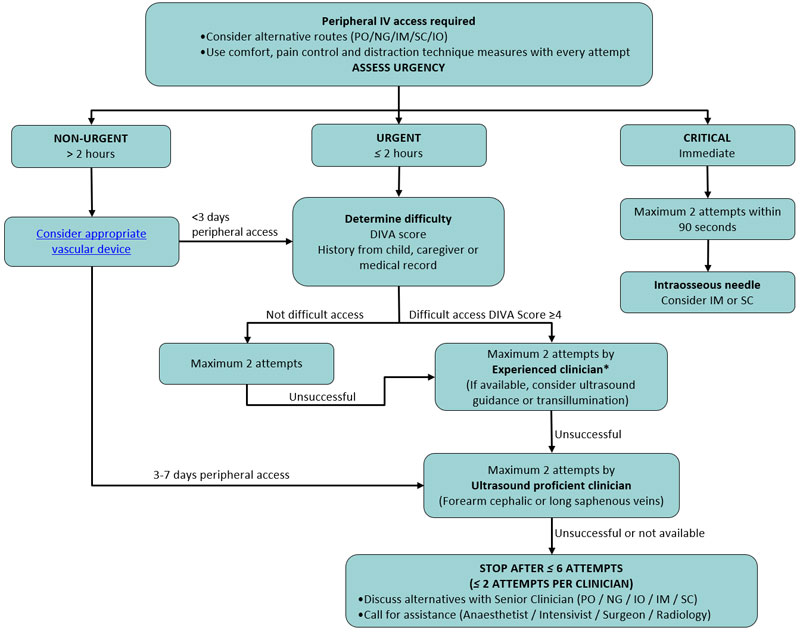
*Experienced Clinician – at least 2 years of acute paediatric experience
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
See video
RCH specific information
For assistance with difficult intravenous access
- 0730 - 1730 (Mon – Fri): Anaesthetics ASCOM 52000
- After hours / public holidays: PICU ASCOM 52327
Last updated September, 2019
Skills Video Drawing Blood From an Picc
Source: https://www.rch.org.au/clinicalguide/guideline_index/Intravenous_access_Peripheral/
Post a Comment for "Skills Video Drawing Blood From an Picc"